“When we cry out for help, they call us crazy. When we speak our truth, they label it paranoia. But what if the real delusion is their refusal to acknowledge our reality?”
– Aremuorin
Introduction: The Mental Health Crisis No One Wants to Talk About
Depression is often misunderstood, but for people of color and minority communities, it’s not just a battle with mental health—it’s a battle against systemic bias, misdiagnosis, and gaslighting. Too often, when Black and Brown individuals report trauma, discrimination, or chronic stress, they are dismissed as “paranoid” or “delusional.” Instead of receiving proper care, they are misdiagnosed with schizophrenia or other psychotic disorders, compounding the very oppression that triggered their distress in the first place.
I haven’t broken the law—yet. But if I get called crazy one more time, I just might start questioning their delusions
This isn’t just anecdotal—it’s a pattern. And it’s killing us.
The Many Faces of Depression: More Than Just Sadness
Depression doesn’t always look like tears and isolation. It can manifest in different ways, especially within communities of color.
1. Major Depressive Disorder (MDD)
A severe and persistent form of depression that lasts for weeks or months, often interfering with daily life. Symptoms include:
• Deep sadness, hopelessness
• Loss of interest in activities
• Fatigue and sleep disturbances
• Suicidal thoughts
2. Persistent Depressive Disorder (Dysthymia)
A long-term, low-grade depression that lasts for years. It may not be as intense as MDD, but it slowly drains joy from life.
3. A typical Depression
Often misdiagnosed in Black and Brown people, this form of depression comes with:
• Mood reactivity (improving when good things happen)
• Increased appetite or weight gain
• Heavy limbs, extreme fatigue
• Sensitivity to rejection (often mistaken for paranoia)
4. Trauma-Induced Depression (PTSD-Related Depression)
For those experiencing racial trauma, police brutality, microaggressions, and workplace discrimination, depression doesn’t exist in a vacuum. It is intertwined with PTSD, leading to:
• Hypervigilance (which may be misinterpreted as paranoia)
• Social withdrawal
• Emotional numbness
• Explosive anger or irritability
5. High-Functioning Depression
Common among professionals, creatives, and activists, this form of depression allows people to “perform” in public while suffering in silence. They may excel at work but crash in private, overwhelmed by exhaustion and despair.
The Cultural Bias in Mental Health: Why Are We Being Misdiagnosed?
Fact: Black people are four times more likely than white people to be diagnosed with schizophrenia—but are no more likely to actually have it. (American Journal of Psychiatry)
Fact: A 2019 study found that Black men with depression are often diagnosed with anger issues instead of mood disorders. (Journal of Racial and Ethnic Health Disparities)
Fact: Black women are less likely to be prescribed antidepressants than white women with the same symptoms. (National Institutes of Health)
The Misdiagnosis Epidemic
Why is this happening? The answer is systemic:
1. Implicit Bias in Psychiatry – Many mental health professionals have been trained to see Black distress as aggression, and our emotional pain as “psychotic” rather than a legitimate response to trauma.
2. Lack of Cultural Competency – Western psychology is based on white, middle-class norms. When we express ourselves differently—through storytelling, spirituality, or strong emotions—it is misunderstood.
3. Over-Pathologizing Black Pain – From slavery to Jim Crow to mass incarceration, Black suffering has been ignored or criminalized. Psychiatry follows this legacy, often treating our distress as a disorder rather than a response to oppression.
4. Gaslighting as a Systemic Tool – When people of color speak out against racism, discrimination, or injustice, they are often labeled as “delusional” or “schizophrenic” rather than being believed.
Historical Case Study: Drapetomania – The ‘Mental Illness’ of Slaves Who Wanted Freedom
In the 1800s, white doctors diagnosed enslaved Africans with drapetomania—a supposed mental illness that caused them to run away. Today, when Black and Brown people resist oppression, they are diagnosed with “delusional disorder.” History is repeating itself.
Depression vs. Delusion: Knowing the Difference
Depression Delusion/Schizophrenia
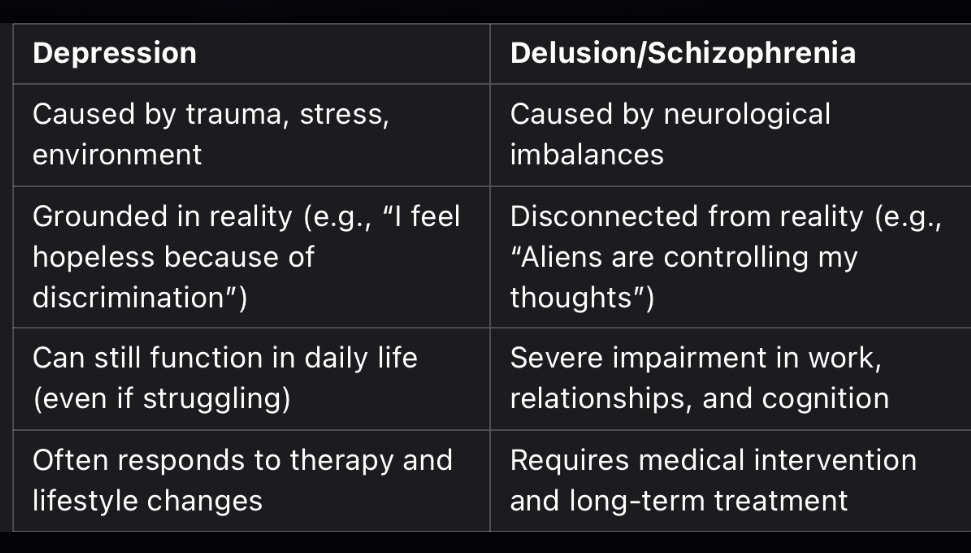
Key takeaway: Just because someone is experiencing trauma-induced distress does not mean they are psychotic. Mislabeling legitimate emotional pain as mental illness is a form of violence.
Solutions: How Do We Fight Back?
1. Demand Culturally Competent Therapy
Find a Black or culturally aware therapist. Platforms like Therapy for Black Girls, Therapy for Black Men, and the Loveland Foundation are good starting points.
2. Document Your Symptoms and Experiences
If you suspect bias in your diagnosis, get a second opinion. Keep a journal of your mental health struggles to show patterns.
3. Educate Ourselves and Our Communities
Mental health is not a weakness. Depression is not “just stress.” The more we understand, the less power the system has over us.
4. Speak Truth to Power
Challenge doctors, therapists, and policymakers on implicit bias in mental health care. Join advocacy groups pushing for systemic change.
The intersection of race and mental health diagnosis reveals significant disparities, particularly concerning the misdiagnosis of mood disorders among Black individuals. Empirical studies have consistently demonstrated that Black patients are disproportionately diagnosed with schizophrenia compared to their white counterparts, even when presenting similar symptoms.
Empirical Evidence of Diagnostic Disparities
A study conducted by Rutgers University found that African Americans with severe depression are more likely to be misdiagnosed as having schizophrenia. The research suggests that clinicians may emphasize psychotic over depressive symptoms in African American patients, leading to skewed diagnoses toward schizophrenia.
Further, the American Psychiatric Association highlights that overdiagnosis of schizophrenia persists among Black populations, potentially due to misinterpretation of cultural expressions and a lack of cultural competence among clinicians.
Socio-Political Context
The American Heart Association defines structural racism as the normalization and legitimization of an array of dynamics—historical, cultural, institutional, and interpersonal—that routinely advantage white people while producing cumulative and chronic adverse outcomes for people of color.
This systemic bias extends into healthcare, where implicit biases and stereotypes influence diagnostic practices. The misdiagnosis of mental health conditions in Black individuals is not merely a medical concern but a reflection of broader socio-political inequities that perpetuate mistrust in healthcare systems and exacerbate mental health disparities.
Professional Insights
Dr. William Lawson, a prominent psychiatrist, has noted that misdiagnosis can lead to inappropriate treatment plans, exacerbating the patient’s condition and contributing to a cycle of mistrust and poor health outcomes.
Addressing these disparities requires a multifaceted approach, including cultural competence training for healthcare providers, systemic reforms to address structural racism, and community engagement to rebuild trust in mental health services.
In summary, the misdiagnosis of depression as schizophrenia in Black individuals is a pressing issue rooted in systemic biases within the healthcare system. Recognizing and addressing these disparities is crucial for ensuring equitable mental health care for all individuals, regardless of race or ethnicity.
Final Thought: We Are Not Crazy—The System Is
It’s time to dismantle the lie that Black and Brown people are “paranoid” when we name our struggles. We are not delusional for recognizing oppression. We are not schizophrenic for feeling the weight of trauma.
We are human. And we deserve care, not condemnation.
#MentalHealthMatters #BlackMentalHealth #DepressionAwareness #EndMisdiagnosis #RacialTrauma #PsychologyBias #WeAreNotDelusional

Aremuorin is a multi-award-winning art artist, writer, and humanitarian, known for his unique fusion of music, writing, and advocacy. With a focus on empowerment and social justice, his work aims to inspire, educate, and uplift communities worldwide. Aremuorin has been honored with numerous accolades, including awards in the UK, USA, and Africa, and holds two honorary doctorate degrees for his contributions to both the arts and humanitarian work. His artistry goes beyond entertainment, as he uses his platform to bring attention to issues of mental health, social change, and cultural pride.
Contact / Mailing List / Linktree / Latest Post / WhatsApp
(C) 2025 Aremuorin – All Rights Reserved
Leave a comment